How Do We Know If Health Care Is Racist?
July 2020 Educational Resources on Racism: Health Equity
The killing of George Floyd on May 25, 2020 sparked weeks of ongoing protests against police brutality, bringing racial justice to the national forefront and inspiring companies, universities and local governments to take action. On June 29, 2020, the Hennepin County Board of Commissioners passed a resolution that declared racism a public health crisis.
Racism is a pervasive, insidious force in U.S. healthcare systems. For starters, African-Americans have never had access to safe, affordable health care in the United States. Before the late 1800s, most communities were tended by a town doctor; if a slave owner/human trafficker was unwilling to pay for a slave's care, they would not receive medical treatment. During the Jim Crow era, white and Black patients and practitioners were separated into different facilities. Today, access is largely determined by health insurance, which can mandate where a patient can go, how many visits they can have and how much it costs them. If someone is uninsured, healthcare expenses often result in bankruptcy.
Access to health care forms the bedrock of equity in the medical industry - and that bedrock is layered with racism. Public health strives for equity by relying on a form of metrics called "social determinants of health" comprised of the environmental conditions in which people are born, live, learn, work, play, worship and age. "These conditions directly affect a wide range of health, functioning, and quality-of-life outcomes and risks," according to the Minnesota Department of Health. Ultimately, society attains health equity if all citizens have access to the same positive outcomes in the conditional environments of their daily lives. Unfortunately, the U.S. faces a long road to achieving genuine health equity.
A lack of entry to the healthcare field also creates a snowball effect of negative outcomes in medicine. For instance, if you only research symptoms or diseases in white bodies, students may not learn how to recognize symptoms or diseases experienced by BIPOC bodies (Big Think). Most often, a greater diversity of representation among medical practitioners proves to be the catalyst for expanding research and new medical practice among non-dominant populations.
According to the Association of American Medical Colleges, only 5% of licensed, practicing doctors identify as Black or African-American as of 2018, whereas 56.2% identify as white/Caucasian.
Similarly, a 2017 study revealed that only 6.2% of registered nurses identify as Black or African-American compared to the whopping 80.8% of nurses who identify as white/Caucasian. Today, almost 60 years after the Civil Rights Movement started, Black Americans still barely see themselves reflected in health care.
Naming racism as a public health crisis is an important first step so that communities can strategically respond, but there are also lesser-known grievances that negatively impact the way that Black and African-American patients experience health care. In particular, most patients who identify as Black, Indigenous or People of Color see their care significantly impacted by the implicit biases of doctors, nurses, receptionists and other medical personnel. Implicit bias is complicated because it is couched in unconscious behaviors, such as reacting favorably or unfavorably to embedded cultural stereotypes and assumptions about a group of people. A 2015 study by the Kirwan Institute for the Study of Race and Ethnicity helpfully identified some of the key characteristics of implicit biases:
- Implicit biases are pervasive. Everyone possesses them, even people with avowed commitments to impartiality such as judges.
- The implicit associations we hold do not necessarily align with our declared beliefs or even reflect stances we would explicitly endorse.
- Implicit biases are malleable. Our brains are incredibly complex, and the implicit associations that we have formed can be gradually unlearned through a variety of de-biasing techniques.
As a direct result of discrimination and implicit bias, people of color in the United States face disparities in access to health care, the quality of care received, and health outcomes. "The attitudes and behaviors of health care providers have been identified as one of many factors that contribute to health disparities," write University of North Carolina, Chapel Hill researchers. For now, researchers know three things:
- Racial discrimination is known to yield poorer health outcomes for Black patients.
- Implicit bias influences why institutional racism persists in health care.
- Federal and state funding allocations will determine how and if Black patients' experiences improve.
Naming racism is an important first step. A public health crisis begets funding to fix the problem and to address a lack of access, lack of representation and personnel's implicit biases. Where will financial support come from for these efforts? Will government agencies, hospitals or insurance companies pay for public health programs aimed at ending racist practices?
The answers remain murky. But one thing is clear: The world is ready for healthcare practices that build equity, create space for compassion and empathy across difference, and ensure that all who need medical treatment feel seen and heard.

Twin Cities PBS is here for you at every stage of learning. Read on to learn how Black Americans are navigating and challenging systematic racism in health care. This month's resources are brought to you by artists, educators, researchers, and illustrators.
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Building Health Equity: Appetite for Change
“I had lost my sixteen-year-old son the previous year to gun violence… I was pulled to do something in the garden related to food, hearing that the universe would do healing for me there.”
Watch time: 6 minutes
Queer Women of Color Ask Who Cares and Who Gets Care?
Whether doctors use abusive language, refuse to acknowledge a patient’s chosen pronouns on medical intake forms or ignore the specific needs of LGBTQ+ patients, normative gender/sexual orientations still abound in the healthcare industry, leaving many with a difficult question: Should I even go to the doctor?
Watch time: 9 minutes
Inequity Is A Matter of Life and Death
Not being white in Minnesota is literally hazardous to your health. Startling gaps in outcomes by race and gender prove that a healthcare system designed by and for one culture isn't working well for others. Public-health experts dive in to understand why, and work with communities to change outcomes and create new possibilities for the future.
Watch time: 6 minutes
How Race Shapes Our Scientists And Our Science

Now a cognitive neuroscientist, Jonathan Jackson has achieved his dream of studying the disease for a living. But he said being a Black scientist has also pushed him down paths he wasn't expecting...“There is some currency in my Black skin for everyone but me," he says.
Read time: 10 minutes
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
COLOR & REFLECT
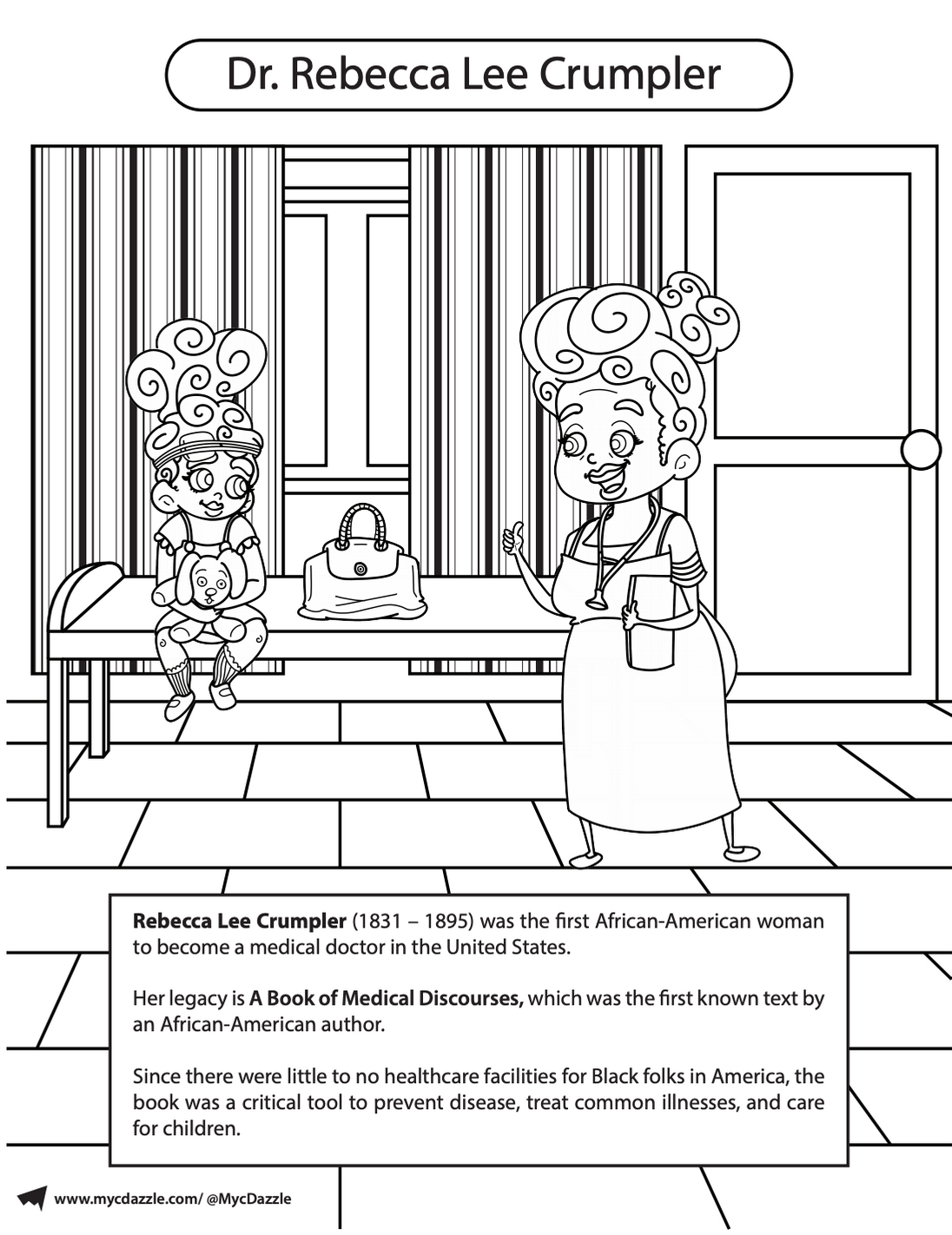
Coloring offers space to reduce anxiety, create focus and bring about more mindfulness. Take time to reflect on what you learned. What surprised you? How do you feel? What questions do you have?
Click here to download this month's coloring page featuring Dr. Rebecca Lee Crumpler.

This educational resource is part of the digital storytelling project Racism Unveiled, which is funded by a grant from the Otto Bremer Trust.
